Discussions on health literacy are increasing as healthcare providers, clinicians, payers and patients consider what this means for healthcare. Having been involved in launching the world’s first digital interactive health channel in the UK in 2000, one thing I learned is not to assume that everyone is alike or has common interests.
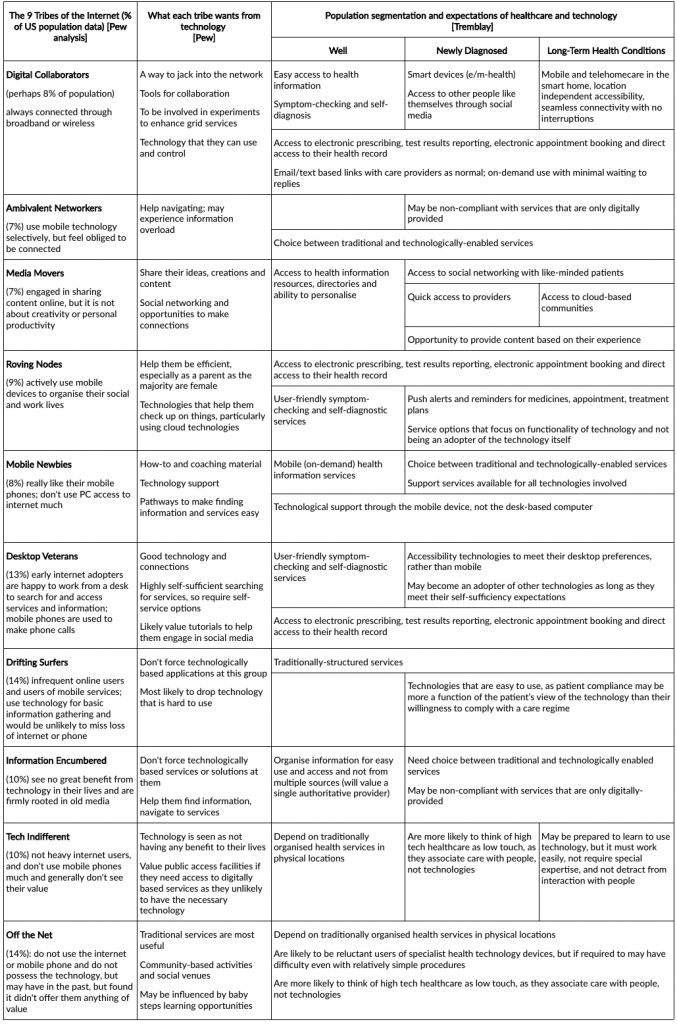
Healthcare systems are poor doing what retailers take for granted, namely the segmentation of their users. When we did the health channel, we worked with a simple framework drawing on work by the California HealthCare Foundation, in their report “Health E-People”. This gave us a workable model of the different types of users and their different needs, and that in developing content and services for them through the Channel, we needed to be mindful of this. More recent work by the Pew Internet Project has identified the “9 Tribes of the Internet”, to reveal how different people interact and use technology. Of course, segmentation can be quite elaborate, but at this stage we need a scaffold to guide our further understanding.
The main assumption we need to make about technology is how it will be used by people and thereby how this informs the adoption/diffusion process. Health and social care are traditionally “high touch” activities, given the way that knowledge has been organised, who knows it and how it is used. This, however, is being challenged by technologies that embody what traditionally has been found in the brains of specialist clinicians — what I call ‘cognologies’.
Increasingly we are seeing technological innovations that can embody both that knowledge (in decision algorithms for instance) and in skill (in robotic devices, vision systems for instance). Will people accept a shift toward high technology care at the expense of its traditional focus on care by humans? Is that an aesthetic preference (we like it) or might people come to prefer “lower touch” technologically-enabled services if it is reliable, and on-demand?
As we think about this, I suggest the following as some thoughts for policy makers and care providers:
- Eventually, the individual will have to own, in some form, their own health record if much of the desired changes in patient behaviours are to be realised. This will lead to patients having a new understanding of information about themselves, and as such this information will need to be clear without mediation or interpretation by others. Patients will, therefore, become involved in decisions about what to do with their information, and with whom it is shared and used; for instance, use in databases whether in commercial or public organisations that will be accountable to the patient for the use of that information. The patient, as what I call the ‘auditor of one’ will come to take a keener interest in the accuracy of the health record and be less tolerant of mistakes or inaccuracies, as is the case in other areas (e.g. banking, credit scoring).
- Not everyone will be digitally enabled in the way technology pundits fantasise about. This is not a digital divide and is not evidence of social exclusion, but is a personal choice of people to lead their lives as they wish in a pluralistic society; it may be that in the end, we all end up as digital natives over time, but some will still be hold-outs, or ‘islands in the net. The key implication here is that service providers will need to move in some cases very slowly to adopt technologies with some types of people. In time, perhaps people may adopt low-level access and interactivity, but for some people technological interactivity will remain at best an option not a preference within an evolving technological ecosystem. It remains to be seen whether this will continue to be the case; evidence from other technologies suggests not, that in time, technologies are broadly universally accepted, but not necessarily used in the same ways by everyone.
- The assessment of benefits of technologies in the traditional health technology assessment [HTA] model will need to pay much greater attention to the segment of the population likely to be involved and the social context of that group, taking account of distinct patterns of use and preferences. This challenges the current paradigm used within HTA communities. The conclusion that one-size-fits-all HTA assessment will increasingly prove inadequate. This means that designing and implementing technologies will need to be far more flexible when it comes to the structure of service delivery as the adoption/diffusion process itself will come to determine the socio-economic benefits. Consider that few today would subject the telephone to an impact assessment – it is now part of our expectations, and we should not be surprised if the same thing happens to evolving technologies in healthcare focused on the use by consumers and patients.
- The tribes model suggests that not everyone will necessarily buy into the technology revolution. For many people, they work in care precisely because they want to have personal contact with people, and not through intermediating technologies. Since many patients also would have that preference, organisations may need to structure services and staffing to ensure the right mix of people to service the right publics. This will challenge approaches to the organisational design of service providers, in the main suggesting more pluralism in variety, scale and function.
- Patient compliance, concordance, adherence may become more dependent on the features of the technologies, their design and ease of use, than on the willingness of the patient to follow a particular care regime. Patients are deliberately non-adherent for many good reasons (some of which reflect fundamental flaws from the medicine itself, its delivery system, or side-effects). Accidental non-adherence is another matter obviously. Helping people understand their limitations in using and working with technologies as matter of personal preferences will become very important, which increases the focus on personalisation.
It is common for health and social care systems, especially where the state is the main source of funding, to tend toward omnibus systems of service delivery, which has difficulty dealing with individual service preferences. Whether it is fully appreciated, such systems favour professional and provider interests and depend on proxy interpretations of patient preference. It would be a mistake to assume a similar approach with technologies. Instead, we should be encouraging approaches which are sensitive to the preferences and usage patterns of individuals. In this way, too, we may actually see services being offered that people will value and use.
The 9 Tribes in Health
Background
Pew Internet Project identified the “9 Tribes of the Internet” in a report in 2009 [http://www.pewinternet.org/2009/06/10/the-nine-tribes-of-the-internet/], to ascertain how different people interact and use technology. The California HealthCare Foundation, in its “Health E-People” [http://www.pewinternet.org/2009/06/10/the-nine-tribes-of-the-internet/], identified three broadly defined populations: the well with an interest in health, the newly diagnosed, and those with long-term or chronic health conditions.
The Pew research was instructive in thinking about how people might deal with a more technologically enabled health and social care system. I have sketched out some relationships in the table which gives an overview of the sort of considerations that are likely relevant and important.
NOTE: This was first written in 2010, and updated in 2019.